Revenue Cycle Management in Medical Billing: Why the Middle of Your Cycle Matters Most

U.S. healthcare spending reached $5.3 trillion in 2024, an 8.2% jump from the previous year, yet nearly 40% of hospitals lost money, with many facing additional financial strain. These numbers expose a troubling paradox. The gap between care delivered and dollars collected continues to widen as payer complexity grows, labor costs climb, and denial rates surge.
For organizations operating on razor-thin margins, closing the gap between care delivered and dollars collected is imperative for survival. The path to stability runs through revenue cycle management in medical billing, and one function matters more than any other coding.
What is Revenue Cycle Management in Medical Billing?
To understand why coding is so key, consider the full revenue cycle. Revenue cycle management in medical billing encompasses the complete financial lifecycle of a patient encounter in a healthcare setting. Every touchpoint, from the initial phone call to the final payment posting, falls under this umbrella. This process unfolds across three distinct phases.
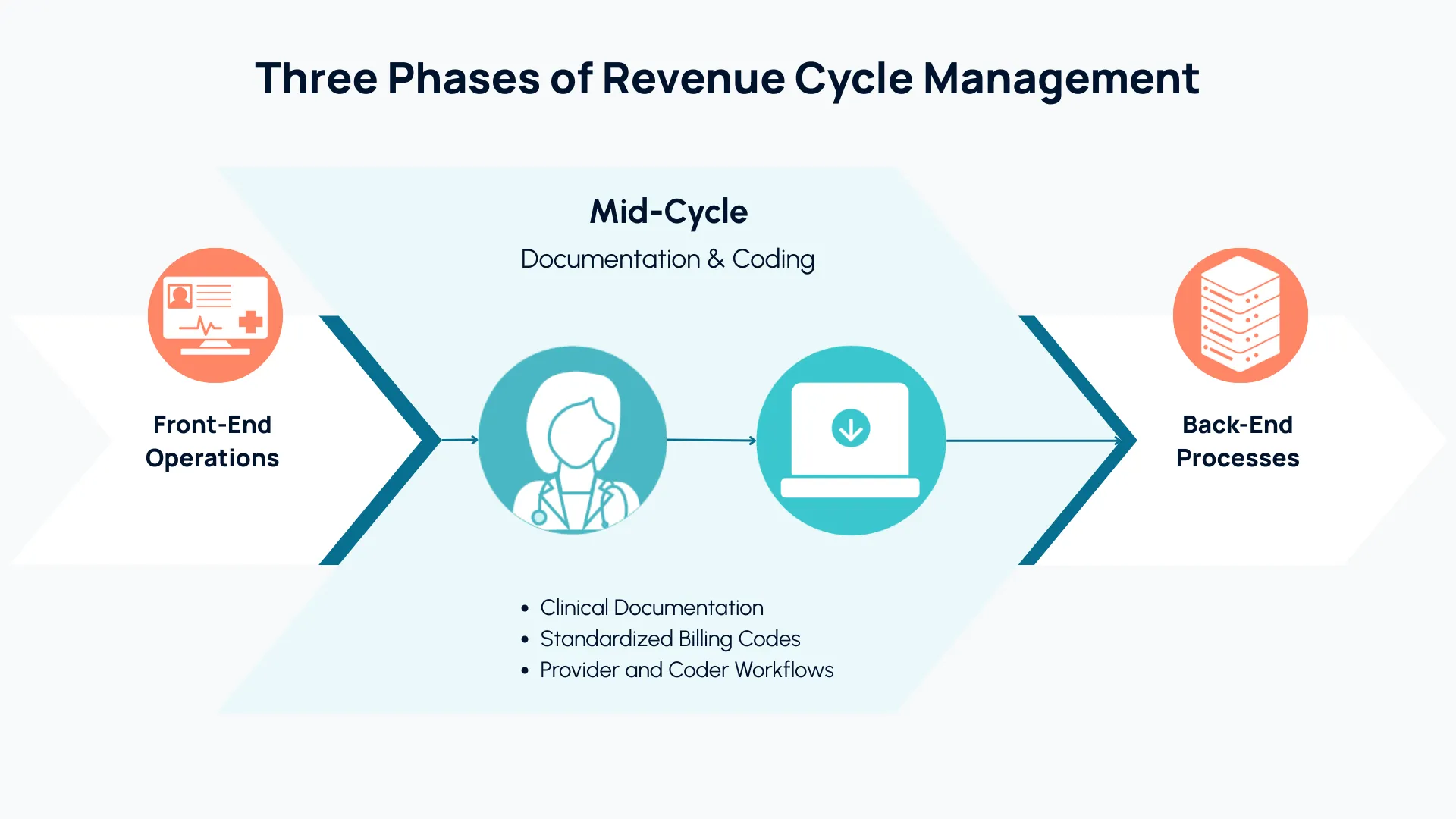
Front-end operations include eligibility verification, scheduling, patient registration, and prior authorization requests.
Mid-cycle functions are the foundation of the medical billing process. They involve clinical documentation, in which patient-provider encounters are documented and translated into standardized alphanumeric billing codes. Every organization splits coding responsibilities differently. In some settings, providers code all of their own charts, and professional coders review only a small portion. In others, professional coders handle a small subset of charts while providers code the majority. Rarely do professionals code every chart. Organizations struggle to hire medical coders, and the economics simply don’t work for high-volume specialties where paying coders to review every encounter would erase already thin margins.
Back-end processes involve claim submission, audits, payment posting, denial management, and collections.
Each phase depends on the one before it, but coding has the greatest influence on financial outcomes and the rest of the RCM cycle. Medical coding connects provider services to the reimbursement that organizations receive. When there are gaps or bottlenecks in coding, the entire revenue cycle management workflow suffers downstream consequences.
Why Coding is Central to Effective RCM?
HealthCare.gov insurers deny almost 20% of in-network claims. Medicare Advantage plans reject nearly 16% on first pass, a $20 billion problem. The trend keeps worsening: 40% of providers now report denial rates exceeding 10%, rising for the third consecutive year. Fighting these denials drains resources, both in the form of time and money. Medical coding inaccuracies and missing CPT/ICD-10 codes cause most denials.
Denials represent just one dimension of coding's financial influence. Coding determines what gets billed, how precisely, how quickly, and whether it satisfies payer requirements. It shapes audit exposure, A/R timelines, and provider administrative burden. No other function touches as many levers.
Accurate coding reduces denials, freeing back-end teams from the grind of appeals. Timely coding also accelerates claim submission, shortens A/R days, and improves cash flow. This is why improving revenue cycle management in medical billing almost always starts with a close look at coding operations.
The Limitations of Traditional Coding Practices
Traditional coding workflows rely heavily on providers and human coders, either employed internally or outsourced. Manual processes worked reasonably well when code sets were smaller and payer requirements were less complex. But now, along with that additional complexity and payer scrutiny, analysts project that patient volumes will increase by 18% in the next 10 years. Outpatient surgery alone will rise by a projected 20% over the same time frame. Manual processes can no longer keep pace.
Computer-assisted coding (CAC) tools emerged as an early solution to streamline medical coding, but they aren’t capable of interpreting free-text physician documentation and offer little transparency into their recommendations. CAC tools still require human review of every chart, which means coders spend their time on repetitive validation rather than strategic work. Meanwhile, physicians spend valuable time managing coding queries and documentation fixes during their off-time, contributing to burnout.
The results of traditional coding practices illustrate core revenue cycle management challenges: extended A/R cycles, elevated denial rates, provider administrative burden, and strained coding teams. This way of doing revenue cycle management in medical billing simply cannot scale to meet the current demand for healthcare.
How Technology Is Transforming RCM?
AI in revenue cycle management has opened up new possibilities that seemed unrealistic just a few short years ago. The emergence of autonomous medical coding, powered by generative AI and large language models, has moved the needle on how to improve revenue cycle management. This new category of revenue cycle automation [LINK] goes far beyond what earlier tools could achieve.
GenAI-native platforms are capable of:
- Interpreting clinical documentation, including free-text physician notes, with near-human fluency.
- Coding most charts independently while routing complex cases to human reviewers with specific guidance about what to verify.
- Integrating directly within EHR systems like Epic or Athena, while preserving existing clinical workflows.
- Using modular reasoning agents to handle distinct aspects of each encounter, such as interpreting clinical ambiguity or mapping symptoms against payer-specific rules.
Coders can now focus their expertise on edge cases and revenue integrity projects rather than grinding through coding routine encounters.
Case in Point: Mercyhealth’s Revenue Turnaround
Mercyhealth achieved 5% revenue uplift and reduced work queue aging by 50% within months of implementing autonomous coding. The multi-regional health system had faced coding backlogs that stalled billing, strained its limited coding team, and created revenue recognition gaps. Patient volumes grew faster than the organization could hire coders.
“Before Arintra, the biggest issue was determining how to handle work with our current staff.”
-Kelly Pierson, Mercyhealth’s Director of Coding and CDI
Arintra's autonomous medical coding solution changed that. The platform's native Epic integration required zero workflow changes for clinical teams. Charts continued moving through familiar processes, with autonomous coding handling routine encounters while routing complex cases for human review.
Mercyhealth established comprehensive coding coverage without adding headcount, enabling its existing team to concentrate on complex cases and revenue integrity initiatives.
"We have given coders the time and opportunity to broaden their knowledge and work at a higher level, and become more important and more needed.”
-Kelly Pierson, Mercyhealth’s Director of Coding and CDI
Arintra’s solution tied every coding decision to clear documentation and reasoning, creating audit trails that satisfied both compliance requirements and external payer scrutiny.
This is revenue cycle transformation in practice: better financial outcomes, stronger compliance, and a redeployed workforce tackling problems that require human judgment.
The ROI of Smarter Revenue Cycle Management
Revenue cycle management optimization via autonomous coding delivers measurable returns across multiple dimensions:
- Faster reimbursement: Accelerated coding compresses the time between service delivery and payment collection, shortening A/R days.
- Reduced denials: Accurate, compliant coding eliminates rework costs and prevents revenue leakage.
- Captured revenue: Organizations recover charges that previously went unrecognized, from missed procedures to diagnosis codes that support medical necessity.
- Operational efficiency: Human coders shift from repetitive work to auditing, provider education, and revenue integrity projects.
- Provider satisfaction: Physicians reclaim time spent on coding queries, and documentation feedback becomes specific and actionable.
For organizations seeking best practices in revenue cycle management, autonomous coding addresses these challenges at their source rather than patching symptoms downstream. The question now is whether your organization is ready to make the shift.
Conclusion: Redefining RCM for the Next Decade
The future of revenue cycle management belongs to organizations that embrace automation at the coding layer. With 40% of hospitals still operating in the red, the margin for error has vanished. Healthcare revenue cycle automation, powered by generative AI, solves the scalability, accuracy, and efficiency challenges that have constrained revenue integrity for decades.
For any organization serious about mastering revenue cycle management in medical billing, coding is the place to start. Health systems that invest in autonomous coding today build the financial resilience healthcare demands for tomorrow.
Ready to Accelerate Revenue Recognition?
Learn how Arintra's autonomous medical coding solution helps leading health systems reduce A/R days, cut denials, and achieve compliant reimbursement, all within the EHR. Book a demo.