Revenue Cycle Management Strategies That Capture Every Dollar Earned
.webp)

The revenue cycle has become something of an arms race, and one side has better weapons. Many insurance companies have automated their claims review processes, while health systems often still rely on manual workflows and overstretched staff to fight for every dollar. This asymmetry shows up in the numbers: denial rates reached nearly 12% in 2024, while hospital operating margins averaged just 1.5%. Payers have modernized, but most hospitals have not.
This financial fragility traces directly back to the revenue cycle in healthcare, the process that determines whether organizations collect payment for the care they deliver. Traditional revenue cycle management approaches are failing under the weight of rising denial rates, staffing shortages, high patient volume, and payer scrutiny that grows more aggressive by the quarter. The old playbook simply cannot keep pace.
Health systems need targeted, technology-enabled revenue cycle management strategies that prioritize efficiency, compliance, adaptability, and revenue integrity. The organizations that embrace this shift will thrive. Those that cling to manual processes will continue fighting the same financial battles with shrinking resources.
Understanding the Modern Revenue Cycle
Most health systems treat revenue cycle management workflow problems as isolated issues. At the front end, registration errors may lead to patient access retraining. In the mid-cycle, coding backlogs prompt urgent hiring pushes. At the back end, a spike in denials triggers a new initiative. Each fix addresses symptoms of revenue leakage problems, while missing the source.
From the moment a patient schedules an appointment to the final payment posting, dozens of handoffs connect registration, coding, billing, and collections into a single financial chain. The relationship between coding and revenue cycle management explains why siloed approaches fail:
- Coding accuracy determines what gets billed
- Coding speed determines when claims go out
- Coding compliance determines whether payers approve or reject claims
A single coding bottleneck doesn't just slow down one department; it cascades forward into denials, backward into documentation requests, and sideways into provider frustration.
Claims adjudication now costs healthcare providers an estimated $25.7 billion annually, according to a survey of 280 hospitals. Roughly 70% of denials eventually get overturned and paid, meaning nearly $18 billion goes toward fighting for revenue that should have been approved the first time.
The Three Pillars of Effective Revenue Cycle Management Strategies
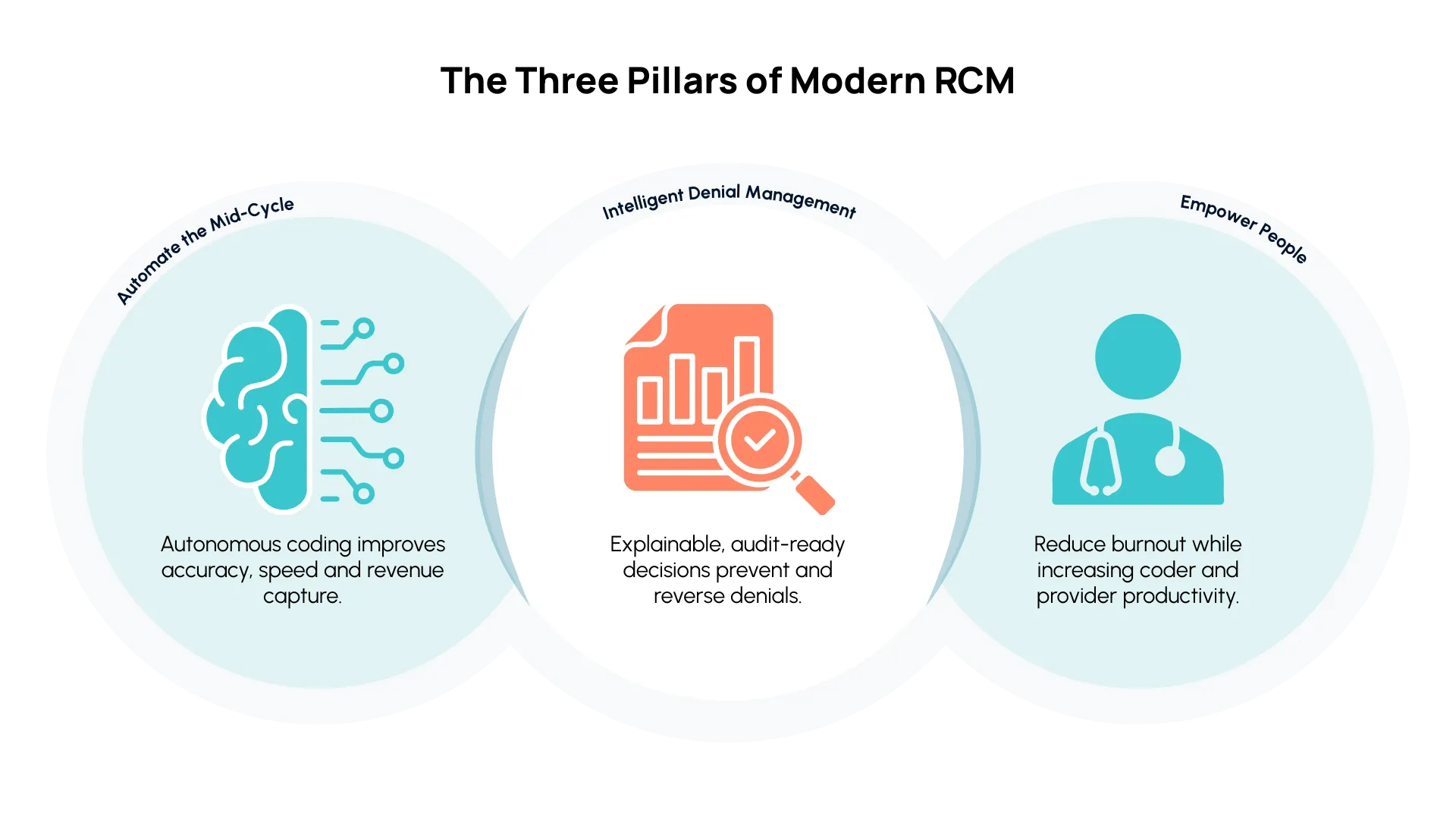
1. Automate the Mid-Cycle for Accuracy and Speed
Understanding medical billing vs. revenue cycle management is important for this conversation. Billing matters, but coding is the function calling the shots. Coding accuracy dictates what gets billed, how quickly claims move, and how much payers actually reimburse. This makes coding the highest-leverage point for intervention, yet most health systems lack the capacity to code effectively.
The Medical Group Management Association reports that 34% of medical groups rank coders as their most difficult revenue cycle role to fill. Training new coders requires hundreds or thousands of hours, and experienced professionals command increasingly competitive salaries. In many outpatient specialties, coders only review about 30% of charts, according to Arintra’s internal data, with the remainder going straight to billing with little oversight because chart volumes are so high.
Healthcare revenue cycle automation through GenAI-powered autonomous coding entirely changes what’s possible. Unlike legacy computer-assisted coding tools that still require human review of every chart, autonomous coding handles routine encounters in minutes, applying payer-specific rules and generating clear decision trails tied to clinical documentation.
Automation works. Arintra’s customers, for example, report the following after implementing autonomous coding:
- 5.1% revenue uplift
- 12% reduction in A/R days
- 43% fewer denials
2. Strengthen Denial Management with Data and Explainability
Payer behavior has shifted dramatically. Initial claim denial rates climbed to 11.8% in 2024, up from 10.2% just a few years earlier. More than half of those denials eventually get reversed on appeal, but each rework costs between $25 and $181 and delays payment. According to KFF's 2024 analysis, fewer than 1% of denied claims ever get formally appealed, meaning most lost revenue stays lost.
AI in revenue cycle management enables a fundamentally different approach. Transparent, audit-ready coding decisions empower revenue cycle teams to challenge denials more effectively. Autonomous coding now leverages historical denial patterns to predict and prevent rejections before submission.
3. Empower People by Reducing Burnout and Raising Productivity
Automation liberates coding staff from days filled with high-volume, repetitive chart processing. Coders freed from routine work can focus on complex cases, clinical documentation improvement initiatives, and revenue integrity projects. Organizations get more from their expertise, and coding is no longer a bottleneck.
Physicians also benefit. The administrative burden of documentation consumes an average of 15.5 hours weekly, with more than half of that time spent on EHR documentation. When autonomous coding catches documentation gaps and provides granular, financially relevant feedback, providers receive actionable guidance that improves their notes over time. Better documentation leads to more accurate coding, fewer denials, and a healthier revenue cycle management strategy across the organization.
Case in Point: Mercyhealth and the ROI of RCM Innovation
The three pillars of modern revenue cycle management strategies converge in Mercyhealth's coding automation implementation: mid-cycle automation, proactive denial management, and workforce empowerment.
This large health system faced the same capacity gap as most organizations: coders reviewed just 30% of ambulatory charts, while the rest went to billing with minimal review. After implementing Arintra's GenAI-powered autonomous coding solution, Mercyhealth achieved:
- 88% direct-to-billing rates
- 50% reduction in aging days
- 5.1% revenue growth
Arintra’s native integration within Epic meant no workflow disruption and no data extraction headaches.
Every coding decision now includes an audit-ready trail that strengthens denial appeals. And the coding team that once spent hours on routine work now focuses on complex cases and revenue integrity, exactly the strategic shift that sustainable RCM demands.
Rethinking RCM for a Sustainable Future
The path forward starts in the mid-cycle. Coding touches revenue recognition, denial rates, and cash flow velocity simultaneously, which is why it delivers ROI faster than almost any other RCM intervention.
Once organizations make this shift, they can stop playing defense and instead:
- Proactively prevent denials
- Deploy coder expertise where it matters
- Free physicians to focus on patients, not paperwork
- Capture every dollar earned for care delivered
- Build more sustainable margins
Health systems finally have what they need to stop losing ground. The organizations moving now are building margins that last, and they're already seeing the results.
Book a demo to discover how autonomous coding can transform your revenue cycle strategy.