What Is Revenue Cycle in Healthcare, and Why Does It Determine Hospital Survival?


Most struggling hospitals don't have a patient volume problem. They have a payment problem due to inefficient reimbursement systems. Healthcare spending hit $5.3 trillion in 2024, but 40% of American hospitals still operate in the red. This financial pressure threatens health systems' ability to sustain their missions and serve their communities.
Fixing these challenges requires understanding how money actually flows through a health system. What is the revenue cycle in healthcare? It's the engine that enables healthcare providers to get paid accurately and timely for the care they’ve delivered. When it operates properly, it enables financial sustainability, however, many organizations are running on fumes.
Understanding and optimizing this process directly reduces A/R days, cuts claim denials, and protects profitability. For healthcare leaders navigating today's financial pressures, mastering revenue cycle management has never been more critical.
What Is the Revenue Cycle in Healthcare?
The revenue cycle spans the entire financial journey of patient care, from the moment someone schedules an appointment to the final payment collection. Three core stages define this workflow:
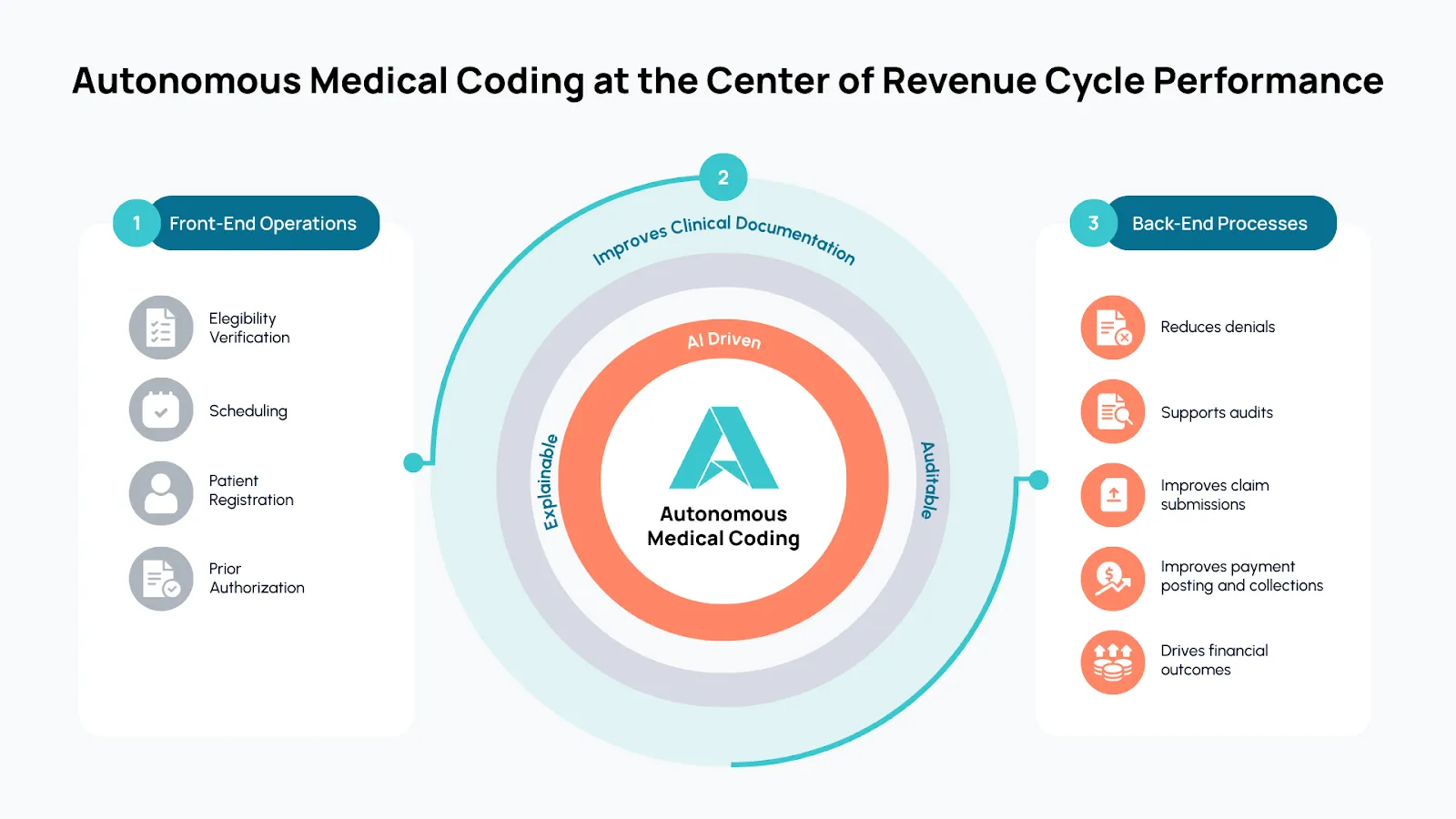
Front-End Operations: This stage includes patient registration, insurance verification, and prior authorization. Staff confirm coverage details and secure approvals before services begin.
Mid-Cycle Functions: This part of the process involves clinical documentation, medical coding, and finally, charge capture. Clinical documentation and medical coding are especially key as they determine reimbursement.
Back-End Processes: The final stage covers claim submission, payment posting, denial management, and collections. Teams submit claims, track payments, and resolve any disputes with payers.
When the revenue cycle management workflow operates efficiently, organizations ensure accurate, timely reimbursement for every service rendered.
Why Revenue Cycle Management Is So Complex
Multiple stakeholders interact throughout the revenue cycle, including providers, coders, payers, IT teams, and compliance officers. At the same time, fragmented processes and disconnected technologies create inefficiencies that compound across the entire system.
The revenue cycle management challenges facing health systems today include rising denial rates, with nearly 15% of claims initially denied according to a survey of hospitals. Half of hospitals and health systems reported more than $100 million in accounts receivable for claims older than six months, while persistent coder shortages and burnout strain overwhelmed teams.
On top of these issues, payers increasingly deploy AI tools for claims adjudication, and 61% of physicians report concerns that this contributes to higher denial rates. Health systems now expect payers to challenge and scrutinize a significant portion of every dollar billed. More than half of denied claims eventually get overturned and paid, but each denial costs between $25 and $181 to rework and appeal.
At the center of all of this complexity sits medical coding.
The Role of Medical Coding in the Revenue Cycle
Coding and revenue cycle management are inseparable. What gets coded, how accurately, and how quickly determines everything downstream.
When coding is accurate and efficient, claims get approved faster, denials drop significantly, and revenue recognition improves. Organizations capture every dollar they earn for the care they deliver.
When coding falls short, revenue leakage grows, compliance risk increases, and physicians face added burden, spending an average of 15.5 hours per week on administration, with more than half of those hours spent on EHR documentation. For many organizations, coding is falling short.
Key Challenges in Traditional Revenue Cycle Processes
Traditional coding processes can't keep pace with modern healthcare volumes. In some specialties, coders review only about 30% of charts, according to Arintra's internal data. The other 70% go to billing with only physician input, creating huge blind spots. A fundamental challenge is that professional coders can't review every chart. Organizations struggle to hire enough of them, and in high-volume specialties, paying coders to touch every encounter would erase already razor-thin margins.
Manual coding bottlenecks slow the entire revenue cycle. Denials and rework costs due to inaccurate coding drain resources, with each denial requiring staff time and attention to appeal. Compliance and audit risks also increase when coding lacks transparency and consistency.
Organizations searching for answers about how to improve revenue cycle management often discover that hiring more coders cannot solve the fundamental capacity problem. The specialized training required for medical coders takes hundreds or thousands of hours.
According to the Medical Group Management Association, 34% of medical groups say coders are the most difficult revenue cycle role to find and hire. The American Medical Association reports a shortage of medical coders nationwide. The coder shortage isn't a hiring problem. It's a capacity problem, and capacity requires a different fix.
How GenAI Is Transforming Revenue Cycle Management
Recent breakthroughs in generative AI have laid the foundation for something that previous automation attempts never achieved: tools that code charts autonomously. Generative AI in revenue cycle management now enables coding directly from unstructured clinical notes.
Unlike computer-assisted coding (CAC) tools that struggle with free-flowing text and require human review of every chart, GenAI-native platforms interpret clinical documentation with human-like fluency. These tools are already transforming the revenue cycle for health systems and physician groups. Arintra’s customers report 5.1% revenue uplift, a 43% reduction in denials, and 12% improvement in A/R days after implementing autonomous coding. Deep integration with EHRs like Epic and Athena ensures seamless adoption without disrupting existing workflows.
Healthcare revenue cycle automation via coding delivers consistency across hundreds of providers. Instead of individual coding approaches that vary by physician, organizations can apply a single, auditable methodology, with coding decisions tied directly to clinical documentation. This uniformity strengthens compliance and makes problems easier to identify and fix.
The Future of the Revenue Cycle: From Automation to Revenue Assurance
The future of revenue cycle management includes automating tasks, but the real change is preventing revenue loss before it happens. Next-generation AI tools integrate autonomous coding, clinical documentation improvement, and denial prevention into unified systems.
In practice, revenue cycle transformation means faster, compliant reimbursement. It means better provider experiences, with physicians reclaiming hours previously spent on administrative tasks. Finally, it means transparent, auditable processes that satisfy both internal compliance requirements and external payer scrutiny.
Ultimately, revenue cycle management optimization in this new era is about capturing every dollar earned while reducing the cost and friction of the revenue cycle itself.
Building a Resilient Revenue Cycle
Back to the original question: what is revenue cycle in healthcare? The answer is clearer now. It's the lever that separates thriving health systems from those fighting to survive, with coding as the fulcrum.
And now, with GenAI-native tools, health systems can secure accurate, compliant reimbursement at scale. Best practices in revenue cycle management should include autonomous coding that handles routine charts in minutes, freeing human coders for complex cases and revenue integrity initiatives.
Through it all, the goals of revenue cycle management remain constant: get paid accurately, quickly, and efficiently for every service delivered. The technology to achieve those goals is finally here.
Ready to transform your revenue cycle? Learn how leading health systems automate coding and accelerate cash flow with Arintra.