Where Does Your Revenue Cycle Management Workflow Break Down?


Where does the money go? U.S. healthcare spending reached $5.3 trillion in 2024, but most hospitals still struggle to break even. Cash on hand sits at a 10-year low. The breakdown happens within the revenue cycle management workflow, where every step determines whether hospitals get paid for the services they’ve rendered. RCM leaders are fighting revenue leakage challenges on three fronts:
- Fragmented workflows spanning multiple teams and technologies
- Chronic shortages of skilled coders
- Payer requirements that shift quarterly
These challenges create persistent gaps between care delivered and payment received. For example, coding delays stall reimbursement, and unworked denials become write-offs. The failures accumulate across handoffs, and the financial impacts compound with each one.
Closing these gaps requires taking a hard look at the entire revenue cycle management workflow. For many organizations, the highest-impact starting point is coding. But understanding the importance of coding requires mapping the full workflow.
What is the Revenue Cycle in Healthcare?
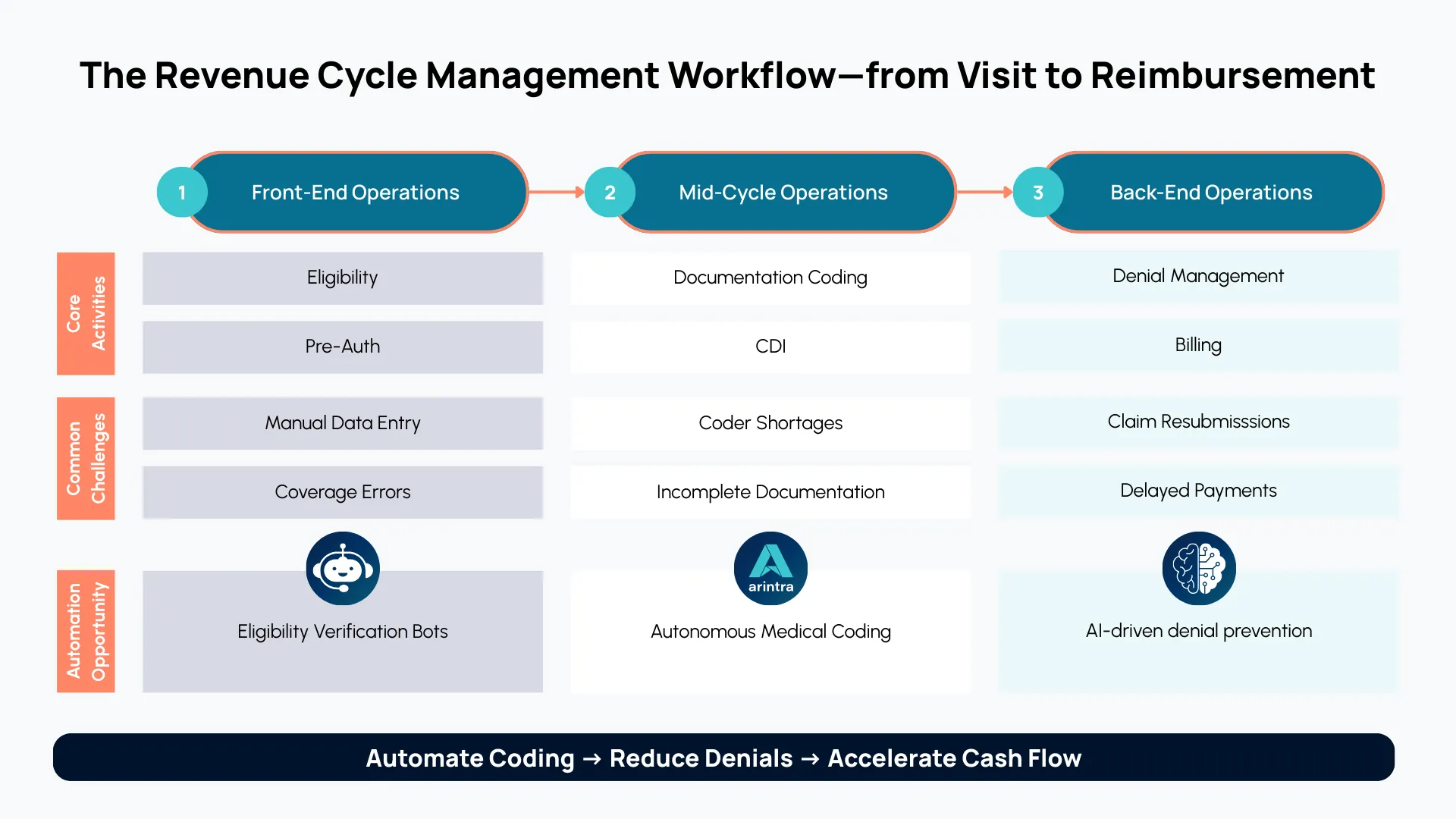
The revenue cycle isn’t a singular process. It involves a series of handoffs, and each one carries risk that can multiply downstream.
The first handoff happens before a patient ever sees their provider. The scheduling team passes the patient’s information to registration, which passes it to the people responsible for insurance verification. An error at this stage can create problems that won’t surface until weeks later, when the claim bounces back in the form of a denial.
The second handoff is perhaps the most critical. After the provider documents their encounter with a patient, someone must translate those clinical notes into billable codes. For many health systems and physician groups, this process involves providers coding their own charts because there simply aren’t enough professional coders to review every patient encounter.
When coding errors occur at this stage, they often trigger denials or compliance flags that require further resources to resolve.
The third handoff involves submitting claims to payers, managing denials, and payment posting. Each handoff creates an opening for errors to compound downstream.
Of the many potential failure points, coding exerts the greatest influence on whether organizations capture the revenue they’ve earned.
Coding: The Hidden Linchpin of RCM
While every phase of revenue cycle management in medical billing carries weight, coding exerts a disproportionate influence on financial outcomes. It often gets less attention than patient-facing registration or high-visibility denials management, but it’s the step that determines whether clinical work becomes recognized revenue.
Timely, accurate coding is what drives first-pass acceptance and shortens days in A/R. Errors and delays, on the other hand, lead to denials, compliance risk, and wasted labor in the form of preventable rework.
The problem is that timely, accurate coding is harder than it sounds because coding challenges are structural:
- Medical group leaders rank coders as the most difficult revenue cycle roles to hire
- Professional coders require hundreds or thousands of hours of specialized training
- In many ambulatory care settings, coders only touch about 30% of charts, according to internal data; providers handle the rest
- Chart volume continues to rise, with projections showing that outpatient volumes will grow 18% over the next decade
This mixed model, where providers code most of their own encounters, introduces major blind spots, including revenue risk and compliance exposure due to inconsistent coding practices.
The math isn’t working out for healthcare organizations as volumes rise, coders remain difficult to hire, and thin margins leave little room for expanded headcount. It’s time to rethink how coding gets done.
Modernizing the RCM Workflow with GenAI
Coding automation tools aren’t new, but their capabilities have changed dramatically. Computer-assisted coding (CAC) emerged in the 1990s and helped coders work faster. Although these tools can suggest codes, they have significant constraints, such as:
- Difficulty understanding unstructured notes
- A lack of transparency in their reasoning
- Requiring human coders to review every decision
That’s changing. AI in revenue cycle management has evolved. Generative AI (GenAI) and large language models (LLMs) power autonomous coding platforms that can:
- Interpret unstructured clinical narratives
- Assign codes without human review on most charts
- Provide transparent reasoning for every decision
This is how Arintra works. Built natively on GenAI, the platform integrates directly with Epic and Athena, accessing a chart's complete clinical context while preserving data integrity. It resolves clinical ambiguity and applies payer-specific rules without disrupting existing workflows.
These capabilities translate into measurable revenue cycle automation results for Arintra’s clients, who report a 12% reduction in A/R days, 43% fewer denials on automated claims, and over 5% revenue uplift through more accurate coding and comprehensive diagnosis capture.
None of this requires replacing coders. It redirects their expertise. Freed from repetitive chart review, coders have time to focus on complex cases, denial appeals, and revenue integrity projects. They move from processing volume to driving strategic impact.
The Payoff: An Efficient, Compliant, and Scalable RCM Workflow
When coding works, everything downstream works better. This is revenue cycle management optimization in practice, and it creates compounding benefits such as:
- Accurate coding that reduces denials
- A reduction in A/R days
- Stable margins that let organizations invest in what matters
Health systems and physician groups deploying autonomous coding achieve these outcomes while also reducing the administrative burden on physicians. Providers spend less time coding charts and answering documentation questions, coders spend less time processing routine charts, and revenue cycle teams spend less time dealing with denials.
For organizations asking how to improve revenue cycle management, the answer increasingly starts with integrating AI into mid-cycle operations. Organizations seeing the strongest results treat coding automation as part of an integrated revenue assurance strategy that also includes clinical documentation improvement and payer-aware denial insights.
The future of revenue cycle management is this integrated model. Organizations that master their revenue cycle management workflow today, with coding as the foundation, position themselves to succeed as volumes grow and payer complexity intensifies.
Ready to streamline your RCM workflow? Book a demo.